Executive Summary
The 2020 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care provides a comprehensive review of evidence-based recommendations for resuscitation and emergency cardiovascular care. The initial guidelines for CPR were published in 1966 by an ad hoc CPR Committee of the Division of Medical Sciences, National Academy of Sciences—National Research Council.1 This occurred in response to requests from several organizations and agencies about the need for standards and guidelines regarding training and response.
Since then, CPR guidelines have been reviewed, updated, and published periodically by the AHA.2–9 In 2015, the process of 5-year updates was transitioned to an online format that uses a continuous evidence evaluation process rather than periodic reviews. This allowed for significant changes in science to be reviewed in an expedited manner and then incorporated directly into the guidelines if deemed appropriate. The intent was that this would increase the potential for more immediate transitions from guidelines to bedside. The approach for this 2020 guidelines document reflects alignment with the International Liaison Committee on Resuscitation (ILCOR) and associated member councils and includes varying levels of evidence reviews specific to the scientific questions considered of greatest clinical significance and new evidence.
Over a half-century after the initial guidelines were published, cardiac arrest remains a leading cause of mortality and morbidity in the United States and other countries worldwide. As reported in the AHA “Heart Disease and Stroke Statistics— 2020 Update,” emergency medical services respond to more than 347 000 adults and more than 7000 children (less than 18 years of age) with out-of-hospital cardiac arrest (OHCA) each year in the United States.10 In-hospital cardiac arrest (IHCA) is estimated to occur in 9.7 per 1000 adult cardiac arrests (approximately 292 000 events annually) and 2.7 pediatric events per 1000 hospitalizations.11 In addition, approximately 1% of newly born infants in the United States need intensive resuscitative measures to restore cardiorespiratory function.12,13
Overall, although both adult and pediatric IHCA outcomes have improved steadily since 2004, similar gains are not being seen in OHCA.10 The proportion of adult patients with return of spontaneous circulation (ROSC) following OHCA that is attended by emergency medical services has remained essentially unchanged since 2012.10
Much of the variation in survival rates is thought to be due to the strength of the Chain of Survival (Figure 1), the critical actions that must occur in rapid succession to maximize the chance of survival from cardiac arrest.14 A sixth link, recovery, has been added to each Chain with this version of the guidelines to emphasize the importance of recovery and survivorship for resuscitation outcomes. Analogous Chains of Survival have also been developed for pediatric OHCA and for both adult and pediatric IHCA. Similarly, successful neonatal resuscitation depends on a continuum of integrated lifesaving steps that begins with careful assessment and and stabilization at the time of birth and through the first 28 days after birth.15
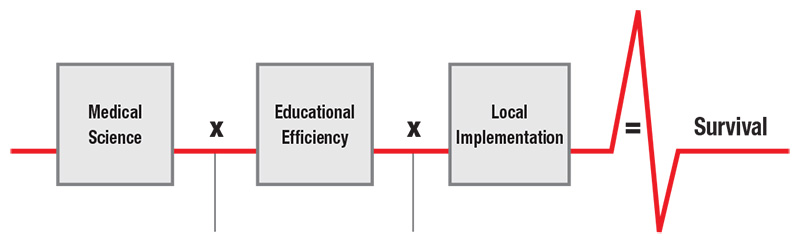
This executive summary provides an overview of and orientation to the 2020 AHA Guidelines, which are organized around the Utstein Formula for Survival (Figure 2).16
Each section in this summary describes the scope of each guideline Part, along with a list of the most significant and impactful new or updated recommendations for that Part. Each section also includes a list of critical knowledge gaps that highlights important research questions and significant opportunities for enhancing the Chain of Survival. This executive summary does not contain extensive external reference citations; the reader is referred to Parts 2 through 7 for more detailed reviews of the scientific evidence and corresponding recommendations.15,17–21
The 2020 Guidelines are based on the extensive evidence evaluation performed in conjunction with ILCOR and the affiliated ILCOR member councils. Three different types of evidence reviews (systematic reviews, scoping reviews, and evidence updates) were used in the 2020 process. Each of these resulted in a description of the literature that facilitated guideline development.23–28 The ILCOR evidence reviews used Grading of Recommendations Assessment, Development, and Evaluation methodology and terminology.29 These AHA treatment recommendations followed standard AHA processes and nomenclature, which are described fully in “Part 2: Evidence Evaluation and Guidelines Development.”19
Each AHA writing group reviewed all relevant and current AHA guidelines for CPR and emergency cardiovascular care,30–41 pertinent 2020 International Consensus on CPR and Emergency Cardiovascular Care Science With Treatment Recommendations evidence evaluations and recommendations,42–48 and all relevant evidence update worksheets to determine whether current guidelines should be reaffirmed, updated, or retired or if new recommendations were needed. The writing groups then drafted, reviewed, and approved recommendations, assigning to each a Class of Recommendation (COR; ie, strength) and Level of Evidence (LOE; ie, quality) (as outlined in Table 3 in Part 2 of this supplement).19
The 2020 Guidelines contain 491 recommendations (Table). Despite recent improvements in support for resuscitation research, 51% of these recommendations are based on limited data and 17% on expert opinion. This highlights the persistent knowledge gaps in resuscitation science that need to be addressed through expanded research initiatives and funding opportunities. With reference to these gaps, we acknowledge the importance of addressing the values and preferences of our key stakeholders: the patients, families, and teams who are involved in the process of resuscitation.
The 2020 Guidelines are organized into knowledge chunks, grouped into discrete modules of information on specific topics or management issues.49 Each modular knowledge chunk includes a table of recommendations, a brief introduction or synopsis, recommendation- specific supportive text, hyperlinked references, and, when relevant, figures, flow diagrams of algorithms, and additional tables.
Abbreviations
| Abbreviation |
Meaning/Phrase |
|---|---|
| ACLS | advanced cardiovascular life support |
| AED | automated external defibrillator |
| AHA | American Heart Association |
| ALS | advanced life support |
| BLS | basic life support |
| COR | Class of Recommendation |
| CPR | cardiopulmonary resuscitation |
| IHCA | in-hospital cardiac arrest |
| ILCOR | International Liaison Committee on Resuscitation |
| LOE | Level of Evidence |
| OHCA | out-of-hospital cardiac arrest |
| PPV | positive-pressure ventilation |
| ROSC | return of spontaneous circulation |
Open table in a new window.
“Part 3: Adult Basic and Advanced Life Support” includes a comprehensive set of recommendations for the care of adult victims of OHCA and IHCA. We reaffirm the critical steps in the Chain of Survival, expand on the postresuscitative care section with the addition of an updated algorithm, and introduce a new link in the Chain of Survival, for recovery and survivorship. The main focus in managing adult cardiac arrest includes rapid recognition, prompt provision of CPR, and defibrillation of ventricular fibrillation and pulseless ventricular tachycardia. Since 2010, the AHA has directed efforts at minimizing the time to provision of chest compressions by focusing the universal sequence of responses on compressions followed by airway and breathing. The 2020 Guidelines continue to highlight the critical importance of chest compressions and leverage current relevant evidence to optimize care and improve survival. Additional recommendations relevant to adult resuscitation appear in “Part 7: Systems of Care.”18
- CPR reaffirmed: Provision of CPR has long been the
hallmark of cardiac arrest management. Updated
evidence from an analysis of over 12 500 patients50
reaffirms the importance of chest compression
quality as well as the following:
- During manual CPR, rescuers should perform chest compressions to a depth of at least 2 inches, or 5 cm, for an average adult while avoiding excessive chest compression depths (greater than 2.4 inches, or 6 cm)(Class 1, LOE B-NR).51–54
- It is reasonable for rescuers to perform chest compressions at a rate of 100 to 120/min (Class 2a, LOE B-NR).50,55
Furthermore, from a new systematic review,44 we recommend that lay rescuers initiate CPR for presumed cardiac arrest because the risk of harm to patients is low if they are not in cardiac arrest (Class 1, LOE C-LD).56–59
- Double sequential defibrillation: Along with CPR, early defibrillation is critical to survival when sudden cardiac arrest is caused by ventricular fibrillation or pulseless ventricular tachycardia. However, rescuers may encounter victims who are refractory to defibrillation attempts. Double sequential defibrillation—shock delivery by 2 defibrillators nearly simultaneously— has emerged as a new technological approach to manage these patients.60–64 At this time, a systematic review reveals that the usefulness of double sequential defibrillation for refractory shockable rhythm has not been established (Class 2b, LOE C-LD).48
- Intravenous (IV) before intraosseous (IO): The peripheral IV route has been the traditional approach for giving emergency pharmacotherapy, although the IO route has grown in popularity and is increasingly implemented as a first-line approach for vascular access. New evidence suggests some uncertainty about the efficacy of the IO route compared with the IV route.65–69 Therefore, it is reasonable for providers to first attempt establishing IV access for drug administration in cardiac arrest (Class 2a, LOE B-NR). IO access may be considered if attempts at IV access are unsuccessful or not feasible (Class 2b, LOE B-NR).
- Early epinephrine administration reaffirmed: In 2 randomized clinical trials,70,71 administration of epinephrine increased ROSC and survival, leading to a recommendation that epinephrine be administered for patients in cardiac arrest (Class 1, LOE B-R).40,72 Uncertainty about the effect of epinephrine on neurological outcome, in addition to the variation in outcomes based on timing and initial rhythm, supported the following new concepts:
- With respect to timing, for cardiac arrest with a nonshockable rhythm, it is reasonable to administer epinephrine as soon as feasible (Class 2a, C-LD).
- With respect to timing, for cardiac arrest with a shockable rhythm, it may be reasonable to administer epinephrine after initial defibrillation attempts have failed (Class 2b, C-LD).
The Adult Cardiac Arrest Algorithm has been updated to emphasize the early administration of epinephrine for patients with nonshockable rhythms.
- Individualized management of resuscitation: Not
all cardiac arrest events are identical, and specialized
management may be critical for optimal
patient outcome, such as when the primary etiology
of arrest is respiratory, a gravid uterus impedes
venous return, or resuscitation involves a viable
fetus. In the Special Circumstances of Resuscitation
section, we highlight 2 such areas (opioid overdose
and cardiac arrest in pregnancy):
- Opioid overdose: The opioid epidemic has resulted in an increase in respiratory and cardiac arrests due to opioid overdose.73 To address this public health crisis, we present 2 new algorithms for the management of opioid-associated emergencies, highlighting that lay rescuers and trained responders should not delay activating emergency response systems while awaiting the patient’s response to naloxone or other interventions (Class 1, LOE E-O). Additionally, for patients known or suspected to be in cardiac arrest, in the absence of a proven benefit from the use of naloxone, standard resuscitative measures should take priority over naloxone administration, with a focus on high-quality CPR (compressions plus ventilation) (Class 1, LOE E-O).73
- Cardiac arrest in pregnancy: We present updated recommendations and a new algorithm highlighting the concept that the best outcomes for both mother and fetus are through successful maternal resuscitation.74 Team planning for cardiac arrest in pregnancy should be done in collaboration with the obstetric, neonatal, emergency, anesthesiology, intensive care, and cardiac arrest services (Class 1, LOE C-LD). Priorities for treating the pregnant woman in cardiac arrest should include provision of high-quality CPR and relief of aortocaval compression through left lateral uterine displacement (Class 1, LOE C-LD). If the pregnant woman with a fundus height at or above the umbilicus has not obtained ROSC with usual resuscitation measures plus manual left lateral uterine displacement, it is advisable to prepare to evacuate the uterus while resuscitation continues (Class 1, LOE C-LD).75–79 To accomplish delivery early, ideally within 5 minutes after the time of arrest, it is reasonable to immediately prepare for perimortem cesarean delivery while initial BLS and advanced cardiovascular life support (ACLS) interventions are being performed (Class 2a, LOE C-EO), although provider skill set and available personnel and resources may also logically influence this timing.74
- Point-of-care ultrasound for prognostication: Many have attempted to leverage the use of new technologies like portable ultrasound machines to provide guidance in making decisions on futility and termination of resuscitation. However, on the basis of a synthesis of the evidence,48 we suggest against the use of point-of-care ultrasound for prognostication during CPR (Class 3: No benefit, LOE C-LD). This recommendation does not preclude the use of ultrasound to identify potentially reversible causes of cardiac arrest or detect ROSC.
- Postresuscitative care: Post–cardiac arrest care, a critical component of the Chain of Survival, demands a comprehensive, structured, multidisciplinary system of care that should be implemented in a consistent manner for the treatment of post– cardiac arrest patients (Class 1, LOE B-NR).40,80 We present a new algorithm that describes the initial stabilization phase and additional emergency activities after ROSC. Key considerations include blood pressure management, monitoring for and treatment of seizures, and targeted temperature management.
- Improving neuroprognostication: Accurate neurological
prognostication in cardiac arrest survivors
who do not regain consciousness with ROSC is
critically important to ensure that patients with
significant potential for recovery are not destined
for certain poor outcomes due to care
withdrawal.81 With updated systematic reviews
on multiple aspects of neuroprognostication,48 in
patients who remain comatose after cardiac arrest,
we recommend that neuroprognostication involve
a multimodal approach and not be based on any
single finding (Class 1, LOE B-NR).48,81 To assist in
this process, we have developed evidence-based
guidance to facilitate multimodal prognostication.
This includes the following:
- In patients who remain comatose after cardiac arrest, we recommend that neuroprognostication be delayed until adequate time has passed to ensure avoidance of confounding by medication effect or a transiently poor examination in the early postinjury period (Class 1, LOE B-NR).82
- In patients who remain comatose after cardiac arrest, it is reasonable to perform multimodal neuroprognostication at a minimum of 72 hours after the return to normothermia, though individual prognostic tests may be obtained earlier than this (Class 2a, LOE B-NR).48
Further, we provide specific guidance on the use of clinical examination, serum biomarkers, electrophysiological tests, and neuroimaging for neuroprognostication.
- Recovery and survivorship: Finally, we have added
an additional link in the Chain of Survival: recovery
from cardiac arrest. Recovery expectations and
survivorship plans that address treatment, surveillance,
and rehabilitation need to be provided
to cardiac arrest survivors and their caregivers
at hospital discharge to address the sequelae of
cardiac arrest and optimize transitions of care to
independent physical, social, emotional, and role
function.83 Recommendations that are critically
important to this concept include the following:
- We recommend structured assessment for anxiety, depression, posttraumatic stress, and fatigue for cardiac arrest survivors and their caregivers (Class 1, LOE B-NR)83–87
- We recommend that cardiac arrest survivors have multimodal rehabilitation assessment and treatment for physical, neurological, cardiopulmonary, and cognitive impairments before discharge from the hospital (Class 1, LOE C-LD).83,88–90
- We recommend that cardiac arrest survivors and their caregivers receive comprehensive, multidisciplinary discharge planning, to include medical and rehabilitative treatment recommendations and return to activity/work expectations (Class 1, LOE C-LD).83
Some of the most pertinent gaps in adult resuscitations research include the following:
- What are optimal strategies to enhance lay rescuer performance of CPR?
- For patients with an arterial line in place, does targeting CPR to a particular blood pressure improve outcomes?
- Can artifact-filtering algorithms for analysis of ECG rhythms during CPR in a real-time clinical setting decrease pauses in chest compressions and improve outcomes?
- Does preshock waveform analysis lead to improved outcome?
- Does double sequential defibrillation and/or alternative defibrillator pad positioning affect outcome in cardiac arrest with shockable rhythm?
- Is the IO route of drug administration safe and efficacious in cardiac arrest, and does efficacy vary by IO site?
- Does epinephrine, when administered early after cardiac arrest, improve survival with favorable neurological outcome?
- Does the use of point-of-care cardiac ultrasound during cardiac arrest improve outcomes?
- Is targeting a specific partial pressure of end-tidal carbon dioxide (ETCO2) value during CPR beneficial, and what degree of rise in ETCO2 indicates ROSC?
- Which populations are most likely to benefit from extracorporeal CPR?
- Does the treatment of nonconvulsive seizures, which are common in postarrest patients, improve patient outcomes?
- Do neuroprotective agents improve favorable neurological outcome after cardiac arrest?
- What is the most efficacious management approach for postarrest cardiogenic shock, including pharmacological, catheter intervention, or implantable device?
- Does targeted temperature management, compared with strict normothermia, improve outcomes?
- What is the optimal duration for targeted temperature management before rewarming?
- What is the best approach to rewarming postarrest patients after treatment with targeted temperature management?
- Are glial fibrillary acidic protein, serum tau protein, and neurofilament light chain measurements valuable for neuroprognostication?
- Do more uniform definitions for status epilepticus, malignant electroencephalogram patterns, and other electroencephalogram patterns enable better comparisons of their prognostic values across studies?
- Is there a consistent threshold value for prognostication for gray-white ratio or apparent diffusion coefficient?
- What do survivor-derived outcome measures of the impact of cardiac arrest survival look like, and how do they differ from current generic or clinician- derived measures?
- Does hospital-based protocolized discharge planning for cardiac arrest survivors improve access to/referral to rehabilitation services or patient outcomes?
- Is there benefit to naloxone administration in patients with opioid-associated cardiac arrest who are receiving CPR with ventilation?
- What is the ideal initial dose of naloxone in a setting where fentanyl and fentanyl analogues are responsible for a large proportion of opioid overdose?
- In cases of suspected opioid overdose managed by a non–healthcare provider who is not capable of reliably checking a pulse, is initiation of CPR beneficial?
- What is the ideal timing of perimortem cesarean delivery for a pregnant woman in cardiac arrest?
- Which patients with cardiac arrest due to “suspected” pulmonary embolism benefit from emergency thrombolysis during resuscitation?
“Part 4 of the 2020 Guidelines, Pediatric Basic and Advanced Life Support” includes recommendations for the treatment of pediatric OHCA and IHCA, including postresuscitation care and survivorship. The causes, treatment, and outcomes of cardiac arrest in children differ from cardiac arrest in adults. For example, pediatric cardiac arrests are more often due to respiratory causes. These guidelines contain recommendations for pediatric BLS and ALS, excluding the newborn period, and are based on the best available resuscitation science. Expansions to pediatric ALS recommendations include care of the child with pulmonary hypertension, congenital heart disease, and post–cardiac arrest recovery. This summary highlights the new and updated recommendations in pediatric BLS and ALS since 2015 that we believe will have a significant impact on process and on patient-related outcomes from cardiac arrest. Additional recommendations related to pediatric resuscitation can be found in “Part 7: Systems of Care.”
- Respiratory rate: Respiratory rates during pediatric CPR have previously been extrapolated from adult data, because of lack of pediatric studies. New data about respiratory rates during CPR in children are now available. Although limited, these data support a higher respiratory rate for children with an advanced airway than was previously recommended.91 When performing CPR in infants and children with an advanced airway, it may be reasonable to target a respiratory rate range of 1 breath every 2 to 3 seconds (20–30 breaths/min), accounting for age and clinical condition. Rates exceeding these recommendations may compromise hemodynamics (Class 2b, LOE C-LD).91 For infants and children with a pulse but absent or inadequate respiratory effort, it is reasonable to give 1 breath every 2 to 3 seconds (20–30 breaths/min) (Class 2a, LOE C-EO).91
- Cuffed endotracheal tubes: Intubation with a cuffed endotracheal tube can improve capnography and ventilation in patients with poor pulmonary compliance and decrease the need for endotracheal tube changes. It is reasonable to choose cuffed endotracheal tubes over uncuffed endotracheal tubes for intubating infants and children (Class 2a, LOE C-LD).92–98
- Cricoid pressure: Although cricoid pressure may be useful in certain circumstances, routine use can impede visualization during laryngoscopy and chest rise with bag-mask ventilation. Clinical studies show that routine use of cricoid pressure reduces the rate of first-attempt intubation success. Routine use of cricoid pressure is not recommended during endotracheal intubation of pediatric patients (Class 3: No benefit, LOE C-LD),99,100 and if cricoid pressure is used, discontinue if it interferes with ventilation or the speed or ease of intubation (Class 3: Harm, LOE C-LD).99,100
- Early epinephrine: The goal of epinephrine administration during CPR is to optimize coronary perfusion pressure and maintain cerebral perfusion pressure. Earlier administration of epinephrine during CPR may increase survival-to-discharge rates. For pediatric patients in any setting, it is reasonable to administer the initial dose of epinephrine within 5 minutes from the start of chest compressions (Class 2a, LOE C-LD).101–104
- Diastolic blood pressure to guide CPR: For patients with continuous invasive arterial blood pressure monitoring in place at the time of cardiac arrest, it is reasonable for providers to use diastolic blood pressure to assess CPR quality (Class 2a, LOE C-LD).105 Although ideal blood pressure targets during CPR are not known, diastolic blood pressure is the main driver of coronary blood flow and may be used to guide interventions if an arterial line is in place.
- Seizures after cardiac arrest: Post–cardiac arrest seizures are common. Many are nonconvulsive, which can be detected only with electroencephalography monitoring. When resources are available, continuous electroencephalography monitoring is recommended for the detection of seizures after cardiac arrest in patients with persistent encephalopathy (Class 1, LOE C-LD).106–109 It is recommended to treat clinical seizures that follow cardiac arrest (Class 1, LOE C-LD).110,111 It is reasonable to treat nonconvulsive status epilepticus that follows cardiac arrest, in consultation with experts (Class 2a, LOE C-EO).110,111
- Recovery and survivorship: New neurological morbidity after cardiac arrest is common and should be addressed with ongoing assessment and intervention to support patients after hospital discharge. It is recommended that pediatric cardiac arrest survivors be evaluated for rehabilitation services (Class 1, LOE C-LD).112–117 It is reasonable to refer pediatric cardiac arrest survivors for ongoing neurological evaluation for at least the first year after cardiac arrest (Class 2a, LOE C-LD).81,83,115,117–122
- Septic shock: Previous AHA guidelines for the management of septic shock included aggressive (20 mL/kg) fluid boluses and lacked additional guidance. In these 2020 Guidelines, a more tailored approach to fluid administration is suggested, and vasopressor recommendations are provided.
- In patients with septic shock, it is reasonable to administer fluid in 10-mL/kg or 20-mL/kg aliquots with frequent reassessment (Class 2a, LOE C-LD).123 Providers should reassess the patient after every fluid bolus to assess for fluid responsiveness and for signs of volume overload (Class 1, LOE C-LD).123–125
- Either isotonic crystalloids or colloids can be effective as the initial fluid choice for resuscitation (Class 2a, LOE B-R).126 Either balanced or unbalanced solutions can be effective as the fluid choice for resuscitation (Class 2a, LOE B-NR).127–129
- In infants and children with fluid-refractory septic shock, it is reasonable to use either epinephrine or norepinephrine as an initial vasoactive infusion (Class 2a, LOE C-LD).130–135
- Opioid overdose: Although most victims of opioid overdose are adults, young children suffer opioid overdose from exploratory behavior, and adolescents through opioid abuse or self-harm exposure. Opioid overdose causes respiratory depression, which can progress to respiratory arrest and then cardiac arrest. Pediatric opioid overdose management is the same as for adults. For a patient with suspected opioid overdose who has a definite pulse but no normal breathing or only gasping (ie, a respiratory arrest), in addition to providing standard pediatric BLS or ALS care, it is reasonable for responders to administer intramuscular or intranasal naloxone (Class 2a, LOE B-NR).136–149 Empirical administration of intramuscular or intranasal naloxone to all unresponsive opioid-associated life-threatening emergency patients may be reasonable as an adjunct to standard first aid and non–healthcare provider BLS protocols (Class 2b, LOE C-EO).137–145,147–150 New opioid-associated emergency algorithms for lay rescuers and healthcare professionals are provided.
Some of the moist pertinent gaps in pediatric resuscitation research include the following:
- What is the optimal route of medication delivery during CPR: IV or IO?
- In what time frame should the first dose of epinephrine be administered during pulseless cardiac arrest?
- With what frequency should subsequent doses of epinephrine be administered?
- With what frequency should the rhythm be checked during CPR?
- What are the optimal chest compression rate and ventilation rate during CPR? Are they age dependent? Do they differ when an advanced airway is in place?
- Are there specific situations in which advanced airway placement is either beneficial or harmful in OHCA or IHCA? Do they differ based on the etiology of cardiac arrest?
- Can echocardiography improve CPR quality or outcomes from cardiac arrest?
- What is the role of extracorporeal CPR for infants and children with OHCA and IHCA due to noncardiac causes?
- What is the optimal timing and dosing of defibrillation for ventricular fibrillation and pulseless ventricular tachycardia?
- What clinical tools can be used to help in the decision to terminate pediatric IHCA and OHCA resuscitation?
- What is the optimal blood pressure target during the post–cardiac arrest period?
- What are the reliable methods for postarrest prognostication?
- What rehabilitation therapies and follow-up should be provided to improve outcomes after cardiac arrest?
- What are the most effective and safe medications for adenosine-refractory supraventricular tachycardia?
“Part 5 of the 2020 Guidelines, Neonatal Life Support”15 includes recommendations on how to follow the algorithm that include anticipation and preparation, umbilical cord management at delivery, initial actions, heart rate monitoring, respiratory support, chest compressions, intravascular access and therapies, withholding and discontinuation of resuscitation, postresuscitation care, and human factors and performance. Consistent with the Utstein Formula for Survival, the 2020 Guidelines provide a comprehensive review of recommendations for neonatal resuscitation, including new and updated recommendations that are based on the latest evidence from studies published in the medical literature and reviews completed by ILCOR.
- Skin-to-skin contact: Placing healthy newborn infants who do not require resuscitation skinto- skin after birth can be effective in improving breastfeeding, temperature control, and blood glucose stability (Class 2a, LOE B-R). A Cochrane systematic review found that healthy infants receiving skin-to-skin contact were more likely to be breastfed at 1 to 4 months of age. In addition, blood glucose after birth was meaningfully higher and cardiorespiratory stability was also improved with skin-to-skin contact.151
- Intubation for meconium: For nonvigorous newborns (presenting with apnea or ineffective breathing effort) delivered through meconium-stained amniotic fluid, routine laryngoscopy, with or without tracheal suctioning, is not recommended (Class 3: No benefit, LOE C-LD). For nonvigorous newborns delivered through meconium-stained amniotic fluid who have evidence of airway obstruction during positive-pressure ventilation (PPV), intubation and tracheal suction can be beneficial (Class 2a, LOE C-EO). Endotracheal suctioning is indicated only if airway obstruction is suspected after providing PPV.46
- Vascular access: For babies requiring vascular access at the time of delivery, the umbilical vein is the recommended route (Class 1, LOE C-EO). If IV access is not feasible, it may be reasonable to use the IO route (Class 2b, LOE C-EO). Babies who have failed to respond to PPV and chest compressions require vascular access to infuse epinephrine and/or volume expanders. Umbilical venous catheterization is the preferred technique in the delivery room.46,152 IO access is an alternative if umbilical venous access is not feasible or care is being provided outside of the delivery room.46
- Termination of resuscitation: In newly born babies receiving resuscitation, if there is no heart rate and all the steps of resuscitation have been performed, cessation of resuscitation efforts should be discussed with the healthcare team and the family. A reasonable time frame for this change in goals of care is around 20 minutes after birth (Class 1, LOE C-LD). Newly born babies who have failed to respond to resuscitative efforts by approximately 20 minutes of age have a low likelihood of survival. For this reason, a time frame for decisions relating to discontinuation of resuscitation efforts is suggested, emphasizing engagement of parents and the resuscitation team before redirecting care.46,153
Some of the most pertinent gaps in neonatal resuscitations research include the following:
- What is the optimal management of the umbilical cord at delivery, especially in the baby who appears to need respiratory support?
- What is the optimal oxygen management at all stages of resuscitation, including when initiating PPV, when providing chest compressions, and after resuscitation?
- What are the optimal dosing, timing, and route of administration for epinephrine?
- What is the optimal management for the detection and treatment of hypovolemia?
- How should neonatal resuscitation be modified in non–delivery room settings?
- What strategies are most effective for optimizing provider and team performance, including training methods, the frequency of retraining intervals, and the approach to briefing, debriefing, and feedback?
- Booster training: It is recommended to implement booster sessions when using a massed learning approach for resuscitation training (Class 1, LOE B-R). Most current resuscitation courses use a massed learning approach: a single training event lasting hours or days coupled with retraining every 1 to 2 years.154 The addition of booster training sessions (ie, brief, frequent sessions focused on repetition of prior content) to resuscitation courses is associated with improved CPR skill retention over 12 months.155–161 The frequency of booster sessions should be balanced against learner attrition (ie, higher attrition rates with more frequent sessions155) and the availability of resources to support implementation of booster training.
- Spaced learning: It is reasonable to use a spaced learning approach in place of a massed learning approach for resuscitation training (Class 2a, LOE B-R).162–164 In contrast to the traditional or massed learning approach involving a 1- or 2-day course, a spaced learning approach separates training into multiple sessions over time, with intervals of weeks to months between sessions. Each spaced session involves the presentation of new content and may include repetition of content from prior sessions.162–164 Two randomized clinical trials in pediatric resuscitation training report that a spaced learning approach results in improved clinical performance and technical skills (IO insertion, bagmask ventilation) in comparison to a traditional 1- or 2-day course.162,164 Because new content and/or skills are presented at each session, learner attendance across all sessions is required to ensure course completion.
- Deliberate practice and mastery learning: Incorporating a deliberate practice and mastery learning model into BLS or ALS courses may be considered for improving skill acquisition and performance (Class 2b, LOE B-NR). Deliberate practice is a training approach where learners are given (1) a discrete goal to achieve, (2) immediate feedback on their performance, and (3) ample time for repetition to improve performance.165 Mastery learning is the use of deliberate-practice training along with testing that uses a set of criteria to define a minimum passing standard that implies mastery of the tasks being learned.166 Studies incorporating a deliberate-practice and mastery-learning model into training demonstrated improved learner performance in resuscitation skills.167–174 Coupling repetition with feedback and allowing sufficient time to achieve competency are key elements associated with improved outcomes.
- In situ simulation training: It is reasonable to conduct in situ simulation-based resuscitation training in addition to traditional training (Class 2a, LOE C-LD). In situ simulation is a form of simulation training activities that occurs in actual patient-care areas.175 One advantage of in situ training is that it provides learners with a more realistic training environment. In situ training can be focused on the development of individual provider technical skills or team-based skills, including communication, leadership, role allocation, and situational awareness.176,177 When added to other educational strategies, in situ training has a positive impact on learning and on performance outcomes.161,164,178–182 The advantages of in situ training should be weighed against the risks of training in clinical spaces.
- Lay rescuer training: A combination of self-instruction and instructor-led teaching with hands-on training is recommended as an alternative to instructor-led courses for lay rescuers. If instructor-led training is not available, self-directed training is recommended for lay rescuers (Class 1, LOE C-LD).183–186 The primary goal of resuscitation training for lay rescuers (ie, non–healthcare professionals) is to increase immediate bystander CPR rates, automated external defibrillator (AED) use, and timely emergency response system activation during an OHCA. Studies comparing self-instruction or video-based instruction with instructor-led training demonstrate no significant differences in performance outcomes.183–186 A shift to more self-directed training may lead to a higher proportion of trained lay rescuers, thus increasing the chances that a trained lay rescuer will be available during OHCA.
- Training school-age children: It is recommended to train middle school– and high school–age children in how to perform high-quality CPR (Class 1, LOE C-LD).187–195 Training school-age children to perform CPR instills confidence and a positive attitude toward responding to an OHCA event.187–195 Targeting this population with CPR training helps to build the future cadre of community-based, trained lay rescuers.
- Disparities in CPR training: Eliminating disparities in CPR training could improve bystander CPR rates and outcomes from cardiac arrest in populations with historically low rates of bystander CPR. Communities with predominantly black and Hispanic populations and those with lower socioeconomic status have lower rates of bystander CPR and CPR training.196–206 It is recommended to target and tailor lay rescuer CPR training to specific racial and ethnic populations and neighborhoods in the United States (Class 1, LOE B-NR).196–200,207–211 It is recommended to target low–socioeconomic status populations and neighborhoods for layperson CPR training and awareness efforts (Class 1, LOE B-NR).201–206,212–215 Targeting training efforts should consider barriers such as language, financial considerations, and poor access to information.
- Barriers to bystander CPR for women: Women are often less likely to receive bystander CPR because rescuers often fear accusations of inappropriate touching, sexual assault, or injuring the victim.216,217 It is reasonable to address barriers to bystander CPR for female victims through educational training and public awareness efforts (Class 2a, LOE C-LD).216–219 Targeted training may help to overcome these barriers and improve bystander CPR rates for female victims.
- Advanced Cardiovascular Life Support course participation: It is reasonable for healthcare professionals to take an adult ACLS course or equivalent training (Class 2a, LOE C-LD).220–228 For more than 3 decades, the ACLS course has been recognized as an essential component of resuscitation training for frontline, acute-care providers. A recent systematic review found that having resuscitation teams with 1 or more team members trained in ACLS results in improved patient outcomes.228 This recommendation supports the use of the ACLS course as foundational training for acute-care providers.
Some of the most pertinent gaps in resuscitation education research include the following:
- Which educational interventions most impact real-world performance and clinical outcomes, as opposed to educational outcomes or performance in training?
- How can instructional design features be combined or blended to optimize outcomes? Future studies should evaluate the synergistic effects of instructional design features when used in a blended manner (eg, in situ simulation training delivered as booster sessions).
- What are the most effective ways to train and develop resuscitation instructors? Future research should evaluate the impact of various faculty development strategies on instructor skills and learner outcomes.
- Summoning willing bystanders: Emergency dispatch systems should alert willing bystanders to nearby events that may require CPR or AED use through mobile phone technology (Class 1, LOE B-NR). Despite the recognized role of lay rescuers in improving OHCA outcomes, most communities experience low rates of bystander CPR and AED use.229,230 Mobile phone technology, such as text messages and mobile phone apps, is available to summon trained members of the general public to nearby events to assist in CPR and to direct those responders to the nearest AED.231 Notification of lay rescuers via a mobile phone app results in improved bystander response times, higher bystander CPR rates, shorter time to defibrillation, and higher rates of survival to hospital discharge.47 As this technology becomes more ubiquitous, studies exploring the impact of these alerts on cardiac arrest outcomes for diverse patient, community, and geographic contexts are needed.
- Cognitive aids and checklists: It may be reasonable to use cognitive aids to improve team performance of healthcare providers during CPR (Class 2b, LOE C-LD). Cognitive aids are prompts designed to help individuals and teams to recall information, complete tasks, and adhere to guideline recommendations.232 Examples include pocket cards, posters, checklists, mobile apps, and mnemonics. Although the use of cognitive aids in trauma resuscitation improves adherence to resuscitation guidelines, reduces errors, and improves survival,233–236 there are no studies evaluating their use by healthcare teams in cardiac arrest.47
- Data for continuous improvement: Continuous improvement starts with disciplined collection and evaluation of data on resuscitation performance and outcomes. It is reasonable for organizations that treat cardiac arrest patients to collect processes-of-care data and outcomes (Class 2a, LOE C-LD). Clinical registries collect information on the processes of care (CPR performance, defibrillation times) and outcomes of care (ROSC, survival) associated with real-world management of cardiac arrest. Registries provide information that can be used to identify opportunities to improve the quality of care. A recent systematic review found improvement in cardiac arrest survival in organizations and communities that implemented cardiac arrest registries.47
Some of the most pertinent gaps in systems of care research include the following:
- Which interventions improve the willingness of the general public to perform CPR and use AEDs, especially for populations and communities with low bystander response rates?
- Does just-in-time AED delivery, including drone delivery of AEDs, increase the number of patients receiving timely defibrillation and improve resuscitation outcomes?
- Which clinical criteria accurately identify patients at increased risk for IHCA?
- What are the ideal components of a hospital rapid response system and rapid response team? How can these factors be integrated into a realistic and effective response model for the prevention of IHCA?
- What is the best structure for individual, team, and system feedback to achieve performance improvement?
- In what settings are community CPR and AED programs cost-effective?
Cardiac arrest remains a condition with considerable morbidity and mortality that broadly affects individuals across age, gender, race, geography, and socioeconomic status. Although there have been modest improvements in survival, there is still considerable work to be done to address the significant burden of this disease. This executive summary provides an overview of new or updated recommendations that are based on rigorous evidence evaluations and included in the 2020 Guidelines.
To continue to make progress toward addressing this condition over the next decade will require further strengthening the Chain of Survival and enhancing coordinated systems of care. Knowledge gaps identified in the 2020 Guidelines point to critically important research questions that should be addressed and that represent opportunities for funding the future trajectory of resuscitation science. Developing guidelines is an important initial step that can advance efforts that will ultimately result in improved outcomes for patients.
- Raina M. Merchant, MD,MSHP
- Alexis A. Topjian, MD, MSCE
- Ashish R. Panchal, MD, PhD
- Adam Cheng, MD
- Khalid Aziz, MBBS, MA, MEd(IT)
- Katherine M. Berg, MD
- Eric J. Lavonas, MD, MS
- David J. Magid, MD, MPH
On behalf of the Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Group
Open table in a new window.
Open table in a new window.
 Login
Login
