Part 7: Systems of Care
Survival after cardiac arrest requires an integrated system of people, training, equipment, and organizations working together to achieve a common goal. Part 7 of the 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care focuses on systems of care, with an emphasis on elements that are relevant to a broad range of resuscitation situations. Previous systems of care guidelines have identified a Chain of Survival, beginning with prevention and early identification of cardiac arrest and proceeding through resuscitation to post–cardiac arrest care. This concept is reinforced by the addition of recovery as an important stage in cardiac arrest survival. Debriefing and other quality improvement strategies were previously mentioned and are now emphasized. Specific to out-of-hospital cardiac arrest, this Part contains recommendations about community initiatives to promote cardiac arrest recognition, cardiopulmonary resuscitation, public access defibrillation, mobile phone technologies to summon first responders, and an enhanced role for emergency telecommunicators. Germane to in-hospital cardiac arrest are recommendations about the recognition and stabilization of hospital patients at risk for developing cardiac arrest. This Part also includes recommendations about clinical debriefing, transport to specialized cardiac arrest centers, organ donation, and performance measurement across the continuum of resuscitation situations.
- Recovery is a critical component of the resuscitation Chain of Survival.
- Efforts to support the ability and willingness of members of the general public to perform cardiopulmonary resuscitation (CPR), and to use an automated external defibrillator, improve resuscitation outcomes in communities.
- Novel methods to use mobile phone technology to alert trained lay rescuers of events requiring CPR have shown promise in some urban communities and deserve more study.
- Emergency system telecommunicators can instruct bystanders to perform hands-only CPR for adults. The No-No-Go framework is effective.
- Early warning scoring systems and rapid response teams can prevent cardiac arrest in both pediatric and adult hospitals, but the literature is too varied to understand what components of these systems are associated with benefit.
- Cognitive aids may improve resuscitation performance by untrained laypersons, but their use results in a delay to starting CPR. More development and study are needed before these systems can be fully endorsed.
- Surprisingly little is known about the effect of cognitive aids on the performance of emergency medical services or hospital-based resuscitation teams.
- Although specialized cardiac arrest centers offer protocols and technology not available at all hospitals, the available literature about their impact on resuscitation outcomes is mixed.
- Team feedback matters. Structured debriefing protocols improve the performance of resuscitation teams in subsequent resuscitation events.
- System-wide feedback matters. Implementing structured data collection and review leads to improved resuscitation processes and survival in both in-hospital and out-of-hospital settings.
Successful resuscitation requires swift and coordinated action by trained providers, each performing an important role within an organizational framework. Willing bystanders, property owners who maintain automated external defibrillators (AEDs), emergency service telecommunicators (also known as dispatchers or call-takers), and basic life support (BLS) and advanced life support (ALS) providers working within emergency medical services (EMS) systems all contribute to successful resuscitation from out-of-hospital cardiac arrest (OHCA). Within the hospital, the work of physicians, nurses, respiratory therapists, pharmacists, and many other professionals supports resuscitation outcomes. Successful resuscitation also depends on the contributions of equipment manufacturers, pharmaceutical companies, resuscitation instructors and instructor trainers, guidelines developers, and many others. Long-term recovery after cardiac arrest requires support from family and professional caregivers, including, in many cases, experts in cognitive, physical, and psychological rehabilitation and recovery. A systems-wide approach to learning and advancing at every level of care, from prevention to recognition to treatment, is essential to achieving successful outcomes after cardiac arrest.
These systems of care guidelines focus on aspects of resuscitation that are broadly applicable to persons of all ages. The guidelines emphasize strategies at every step in the continuum of care to improve cardiac arrest survival: to increase the proportion of patients with OHCA who receive prompt cardiopulmonary resuscitation (CPR) and early defibrillation; to prevent in-hospital cardiac arrest (IHCA); and to examine the use of cognitive aids to improve resuscitation team performance, the role of specialized cardiac arrest centers, organ donation, and measures to improve resuscitation team performance and resuscitation outcomes.
These guidelines are designed primarily for North American healthcare providers who are looking for an up-to-date summary for clinical care and the design and operation of resuscitation systems, as well as for those who are seeking more in-depth information on resuscitation science and gaps in current knowledge. The emphasis in this Part of the 2020 American Heart Association (AHA) Guidelines for CPR and Emergency Cardiovascular Care (ECC) is on elements of care involving coordination between different contributors to the Chain of Survival (eg, emergency telecommunicators and untrained lay rescuers), those elements common to the resuscitation of different populations (eg, community CPR training and public access to defibrillation, early interventions to prevent IHCA), and means to improve the performance of resuscitation teams and systems.
Some recommendations are directly relevant to lay rescuers who may or may not have received CPR training and who have little or no access to resuscitation equipment. Other recommendations are relevant to persons with more advanced resuscitation training, functioning either with or without access to resuscitation drugs and devices, working either within or outside of a hospital. Recommendations for actions by emergency telecommunicators who provide instructions before the arrival of EMS are provided. Some treatment recommendations involve medical care and decision-making after return of spontaneous circulation (ROSC) or after resuscitation has been unsuccessful. Importantly, recommendations are provided related to team debriefing and systematic feedback to increase future resuscitation success.
Coronavirus Disease 2019 (COVID-19) Guidance
Together with other professional societies, the AHA has provided interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19 infection. Because evidence and guidance are evolving with the COVID-19 situation, this interim guidance is maintained separately from the ECC guidelines. Readers are directed to the AHA CPR and ECC website (cpr.heart.org) for the most recent guidance.1
The Systems of Care Writing Group included a diverse group of experts with backgrounds in clinical medicine, education, research, and public health. Because the systems of care guidelines draw material from each of the main writing groups, the Chairs of each writing group collaborated to develop the systems of care guidelines along with content experts, AHA staff, and the AHA Senior Science Editors. Each recommendation was developed and formally approved by the writing group from which it originated.
The AHA has rigorous conflict of interest policies and procedures to minimize the risk of bias or improper influence during the development of guidelines. Prior to appointment, writing group members disclosed all commercial relationships and other potential (including intellectual) conflicts. These procedures are described more fully in “Part 2: Evidence Evaluation and Guidelines Development.”2 Disclosure information for writing group members is listed in Appendix 1.
These systems of care guidelines are based on the extensive evidence evaluation performed in conjunction with the International Liaison Committee on Resuscitation (ILCOR) and affiliated ILCOR member councils. Three different types of evidence reviews (systematic reviews, scoping reviews, and evidence updates) were used in the 2020 process. Each of these resulted in a description of the literature that facilitated guideline development. A more comprehensive description of these methods is provided in “Part 2: Evidence Evaluation and Guidelines Development.”2
As with all AHA guidelines, each 2020 recommendation is assigned a Class of Recommendation (COR) based on the strength and consistency of the evidence, alternative treatment options, and the impact on patients and society. The Level of Evidence (LOE) is based on the quality, quantity, relevance, and consistency of the available evidence (Table 1).
For each recommendation in “Part 7: Systems of Care,” the originating writing group discussed and approved specific recommendation wording and the COR and LOE assignments. In determining the COR, the writing group considered the LOE and other factors, including systems issues, economic factors, and ethical factors such as equity, acceptability, and feasibility. These evidence-review methods, including specific criteria used to determine COR and LOE, are described more fully in “Part 2: Evidence Evaluation and Guidelines Development.”2 The Systems of Care Writing Group members had final authority over and formally approved these recommendations.
Open table in a new window
The 2020 guidelines are organized into “knowledge chunks,” grouped into discrete modules of information on specific topics or management issues.3 Each modular knowledge chunk includes a table of recommendations that uses standard AHA nomenclature of COR and LOE. A brief introduction or short synopsis is provided to put the recommendations into context with important background information and overarching management or treatment concepts. Recommendation-specific text clarifies the rationale and key study data supporting the recommendations. When appropriate, flow diagrams or additional tables are included. Hyperlinked references are provided to facilitate quick access and review.
Each 2020 AHA Guidelines for CPR and ECC document was submitted for blinded peer review to 5 subject matter experts nominated by the AHA. Before appointment, all peer reviewers were required to disclose relationships with industry and any other potential conflicts of interest, and all disclosures were reviewed by AHA staff. Peer reviewer feedback was provided for guidelines in draft format and again in final format. All guidelines were reviewed and approved for publication by the AHA Science Advisory and Coordinating Committee and AHA Executive Committee. Disclosure information for peer reviewers is listed in Appendix 2.
| Abbreviation | Meaning/Phrase |
|---|---|
| ALS | advanced life support |
| AED | automated external defibrillator |
| AHA | American Heart Association |
| BLS | basic life support |
| CAC | cardiac arrest center |
| COR | Class of Recommendation |
| CPR | cardiopulmonary resuscitation |
| EMS | emergency medical services |
| IHCA | in-hospital cardiac arrest |
| ILCOR | International Liaison Committee on Resuscitation |
| LOE | Level of Evidence |
| MET | medical emergency team |
| OHCA | out-of-hospital cardiac arrest |
| OR | odds ratio |
| PAD | public access defibrillation |
| RCT | randomized controlled trial |
| ROSC | return of spontaneous circulation |
| RR, aRR | relative risk, adjusted relative risk |
| RRT | rapid response team |
| T-CPR | telecommunicator CPR instructions |
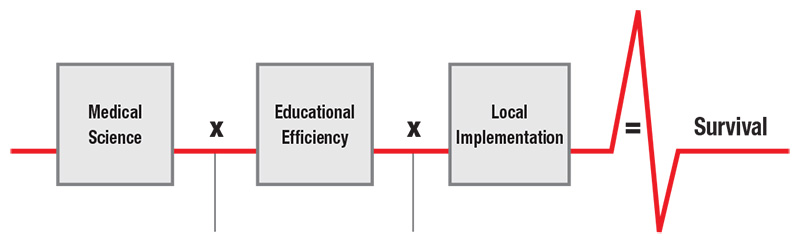
The development and implementation of resuscitation systems of care is founded on the Utstein Formula for Survival.1 The Utstein Formula holds that resuscitation survival is based on synergy achieved by the development and dissemination of medical science (ie, resuscitation guidelines based on the best available evidence); educational efficiency, which includes the effective training of resuscitation providers and members of the general public; and local implementation, which includes seamless collaboration between caregivers involved in all stages of resuscitation and post–cardiac arrest care (Figure 1). Parts 3 through 5 of the 2020 Guidelines represent the AHA’s creation of guidelines based on the best available resuscitation science. In “Part 6: Resuscitation Education Science,” the AHA critically evaluates the science of training medical professionals and the general public to assist a person in cardiac arrest. In “Part 7: Systems of Care,” we explore resuscitation topics that are common to the resuscitation of infants, children, and adults.
Since 1991, the AHA has emphasized the concept of a chain of survival, the coordinated effort used to implement resuscitation science and training.2 With minor variations for the BLS, ALS, and pediatric ALS care settings, the AHA’s Chain of Survival emphasized early recognition of cardiac arrest, activation of the emergency response system, early defibrillation, high quality CPR, advanced resuscitation techniques, and post–cardiac arrest care.
Several improvements have been made to the Chain of Survival concept in these guidelines. Because the causes and treatment of cardiac arrest differ between adults and infants/children as well as between IHCA and OHCA, specific Chains of Survival have been created for different age groups and situations (Figure 2). Each chain has also been lengthened by adding a link for recovery. The neonatal Chain of Survival concept (not supported by a graphic) differs somewhat, because there are far greater opportunities for community and facility preparation before birth, and neonatal resuscitation teams can anticipate and prepare with advance warning and parental involvement. However, the principles of the Chain of Survival and the formula for survival may be universally applied. This Part focuses on recommendations for broad interventions along the entire Chain of Survival that can improve outcomes for all rather than for merely one patient.
Although there are intentional differences in content and sequence due to populations and context, each Chain of Survival includes elements of the following:
- Prevention and preparedness, including responder training, early recognition of cardiac arrest, and rapid response
- Activation of the emergency response system, either outside of or within the hospital
- High-quality CPR, including early defibrillation of ventricular fibrillation and pulseless ventricular tachycardia
- Advanced resuscitation interventions, including medications, advanced airway interventions, and extracorporeal CPR
- Post–cardiac arrest care, including critical care interventions and targeted temperature management
- Recovery, including effective support for physical, cognitive, emotional, and family needs
Prevention of cardiac arrest in the out-of-hospital setting includes measures to improve the health of communities and individuals as well as public awareness campaigns to help people recognize the signs and symptoms of acute coronary syndromes and cardiac arrest. In the hospital setting, preparedness includes early recognition of and response to the patient who may need resuscitation (including preparation for high-risk deliveries), rapid response teams (see Prevention of IHCA), and training of individuals and resuscitation teams. Extensive information about individual and team training is also provided in “Part 6: Resuscitation Education Science.”3 Emergency response system development, layperson and dispatcher training in the recognition of cardiac arrest, community CPR training, widespread AED availability, and telecommunicator instructions that enable members of the general public to initiate high-quality CPR and perform early defibrillation are all important components of this step in the out-of-hospital setting. Recent innovations include using mobile phone technology to summon members of the public who are trained in CPR (see Mobile Phone Technologies to Alert Bystanders of Events Requiring CPR). As described in “Part 5: Neonatal Resuscitation,” predelivery preparedness is an essential component of successful neonatal resuscitation.4
Activation of the emergency response system typically begins with shouting for nearby help. Outside the hospital, immediate next steps include phoning the universal emergency response number (eg, 9-1-1) and sending someone to get the nearest AED. For IHCA, parallel steps include summoning the hospital’s resuscitation team.
High-quality CPR, with minimal interruptions and continuous monitoring of CPR quality, and early defibrillation of ventricular fibrillation and pulseless ventricular tachycardia together form the cornerstone of modern resuscitation and are the interventions most closely related to good resuscitation outcomes. Importantly, these time-sensitive interventions can be provided by members of the public as well as by healthcare professionals. Similarly, in cases of opioid-associated respiratory arrest, early administration of naloxone by bystanders or trained rescuers can be lifesaving.
Advanced resuscitation interventions, including pharmacotherapy, advanced airway interventions (endotracheal intubation or supraglottic airway placement), and extracorporeal CPR may also improve outcomes in specific resuscitation situations.
Post–cardiac arrest care includes routine critical care support (eg, mechanical ventilation, intravenous vasopressors) and also specific, evidence-based interventions that improve outcomes in patients who achieve ROSC after successful resuscitation, such as targeted temperature management. Specific recommendations for targeted temperature management are found in Parts 3, 4, and 5, which provide the 2020 AHA adult,5 pediatric,6 and neonatal guidelines,4 respectively. Because there is no earlier method to reliably identify patients in whom a poor neurological outcome is inevitable, current guidelines for adults recommend against withdrawal of life support for at least 72 hours after resuscitation and rewarming from any induced hypothermia, and perhaps longer.5,8,9 A great deal of active research is underway to develop additional neuroprotective strategies and biomarkers to indicate a good, or poor, prognosis after ROSC.
Recovery from cardiac arrest continues long after hospital discharge. Depending on the outcome achieved, important elements of recovery may include measures to address the underlying cause of cardiac arrest, secondary-prevention cardiac rehabilitation, neurologically focused rehabilitative care, and psychological support for the patient and family. A growing and important body of research examines interventions to benefit the cardiac arrest survivor.10
Although the Chain of Survival emphasizes key elements in the care of an individual patient, it does not sufficiently emphasize steps that are necessary for improving future performance. Examples include conducting a structured team debriefing after a resuscitation event, responding to data on IHCAs collected through the AHA’s Get With The Guidelines initiative, and reviewing data collected for OHCA by using the Utstein framework (Table 2). Several formal process-improvement frameworks, including Lean, Six Sigma, the High Reliability Organization framework, and the Deming Model for Improvement, exist to facilitate continuous improvement. The AHA and other organizations have recommended structures for specific performance-improvement initiatives in resuscitation. The goal is to become a “learning healthcare system”11 that uses data to continually improve preparedness and resuscitation outcomes. Application of this concept to resuscitation systems of care has been previously supported, and is ongoing in many resuscitation organizations.12,13
| Table 2. Examples of the Use of Data for Systems Improvement |
|---|
| After reading about the role of AEDs in the workplace, the manager of a busy office building installed an AED and obtained hands-only CPR training for all of her staff. |
| In response to data that showed a large number of opioid overdoses at the main branch of the public library, an EMS agency provided library staff with naloxone kits and training. |
| During resuscitation, the Team Leader identified that the rescuer who was providing bag-mask ventilation via endotracheal tube was hyperventilating the patient. The Team Leader coached the rescuer to compress the bag only enough to achieve chest rise. |
| In response to data showing low bystander CPR rates in some neighborhoods, free CPR classes were provided in community centers in those neighborhoods. |
| During the team debriefing after a difficult but successful pediatric resuscitation, an error in epinephrine dosing was discovered. The root cause was traced to the need to calculate drug volume under pressure. A reference book was created, listing standard resuscitation medication volumes in milliliters for children of different weights. |
| In response to research showing that women who are victims of cardiac arrest are less likely than men to receive bystander CPR, focus groups were held to identify the root causes for this reluctance, and training was adjusted to target these barriers. |
| In response to data showing that many newly born infants became hypothermic during resuscitation, a predelivery checklist was introduced to ensure that steps were carried out to prevent this complication. |
| AED indicates automated external defibrillator; CPR, cardiopulmonary resuscitation; and EMS, emergency medical services. |
For OHCA, major contributors to resuscitation success are early and effective CPR and early defibrillation. Measures to reduce delays to CPR, improve the effectiveness of that CPR, and ensure early defibrillation for patients with shockable rhythms are therefore a major component of these guidelines.
For IHCA, the major contributors to resuscitation success are similar, but the presence of healthcare professionals affords the opportunity to prevent cardiac arrest. The median time from hospital admission to IHCA in adult patients is 2 days.15 Early identification of the decompensating patient may allow for stabilization that prevents cardiac arrest. This intervention includes 2 steps: identifying the patient at risk, and providing early intervention, either by the patient’s current caregivers or by members of a dedicated team, to prevent deterioration. Because there are separate adult and pediatric evidence bases for these questions, the Adult Basic and Advanced Life Support Writing Group and the Pediatric Basic and Advanced Life Support Writing Group performed parallel evaluations of the evidence about early warning scoring systems as well as about rapid response teams (RRTs) and medical emergency teams (METs).
| COR | LOE | Recommendation |
|---|---|---|
| 2b | C-LD |
|
Synopsis
CPR and AED use are lifesaving interventions, but rates of bystander action are low.13 Mass media campaigns (eg, advertisements, mass distribution of educational materials), instructor-led training (ie, instructor-facilitated CPR training in small or large groups), and various types of bundled interventions have all been studied to improve rates of bystander CPR in communities.1–12 Bundled interventions include multipronged approaches to enhancing several links in the Chain of Survival, involving targeted (based on postal code or risk assessment) or untargeted (mass) instruction incorporating instructors, peers, digital media (ie, video), or self-instruction. Depending on the context, community could refer to a group of neighborhoods; 1 or more cities, towns, or regions; or a whole nation.14
Recommendation-Specific Supportive Text
- A 2020 ILCOR systematic review14 identified 1 randomized controlled trial (RCT)15 and 16 observational studies1–12,16–19 reporting bystander CPR rates and/or survival outcomes. Bystander CPR rates improved in 12 of these studies.1–12
Instructor-Led Training: Six observational studies assessed the impact of instructor-led training.1–4,17–19 Two of 4 studies found improvement in survival with good neurological outcomes after implementation of instructor-led training.1,2,17,18 Two of 3 studies reported improvements in survival to hospital discharge,1,3,18 and 1 study demonstrated an improvement in ROSC after instructor-led training.3 Instructor-led training improved bystander CPR rates by 10% to 19% in 4 studies.1–4
Mass Media Campaigns: One observational study reported a 12% absolute increase in bystander CPR rates after a campaign of television advertisements promoting bystander CPR.6 However, mass distribution (via mail) of a 10-minute CPR instructional video to 8659 households resulted in no significant improvement in bystander CPR rates when compared with a community with households that did not receive a video (47% in intervention households, 53% in controls).15
Bundled Interventions: Nine observational studies evaluated the impact of bundled interventions on bystander CPR rates and survival outcomes.5,7–12,16,19 Bystander CPR rates were improved in 7 of these studies.4,5,7–12,16
These recommendations were created by the AHA Resuscitation Education Science Writing Group and are supported by a 2020 ILCOR systematic review.14
| COR | LOE | Recommendation |
|---|---|---|
| 1 | B-NR |
|
Synopsis
Early defibrillation significantly increases survival rates from OHCA.34–37 Public access defibrillation (PAD) programs are designed to reduce the time to defibrillation by placing AEDs in public places and training members of the public to use them. Compared with traditional EMS systems without a PAD program, persons who experience an OHCA in EMS systems with a PAD program have higher rates of ROSC; higher rates of survival to hospital discharge and at 30 days after OHCA; and higher rates of survival with favorable neurological outcome at hospital discharge, at 30 days, and at 1 year after OHCA.9,10,33 On the basis of this evidence, we recommend that PAD be implemented in communities with individuals at risk for cardiac arrest (eg, office buildings, casinos, apartment buildings, public gatherings). Although the existing evidence supports the effectiveness of PAD programs, the use of public access defibrillators by lay rescuers remains low.38,39 Additional research is needed on strategies to improve public access defibrillation by lay rescuers, including the role of the emergency medical dispatcher in identifying the nearest AED and alerting callers to its location, the optimal placement of AEDs, and the use of technology to enhance rescuers’ ability to deliver timely defibrillation.33,40
Recommendation-Specific Supportive Text
- Of 31 studies that assessed the impact of PAD programs, 27 (1 RCT20 and 26 observational studies1–3,5,7,8,11–19,21–23,25–28,30–32,41 found improved outcomes while 4 observational studies4,6,24,29 found no difference in outcomes.
A 2020 ILCOR systematic review33 found low-quality evidence of improved survival with favorable neurological outcome for systems with a PAD program compared with those without a program, at 1 year from 1 observational study4 enrolling 62 patients (43% versus 0%, P=0.02), at 30 days from 7 observational studies3,22,25,26,29,30,41 enrolling 43116 patients (odds ratio [OR], 6.60; 95% CI 3.54–12.28), and at hospital discharge from 8 observational studies1,2,4,7,11–13,24 enrolling 11837 patients (OR, 2.89; 95% CI, 1.79–4.66).
This same review found low- to moderate-quality evidence of improved survival for systems with a PAD program compared with those without a program, at 30 days from 8 observational studies3,5,15,17,22,28–30 enrolling 85589 patients (OR, 3.66; 95% CI, 2.63–5.11) and at hospital discharge from 1 RCT20 enrolling 235 patients (RR, 2.0; 95% CI, 1.07–3.77) and 16 observational studies1,2,6–8,11,13,14,16,18,19,21,24,27,31,32 enrolling 40243 patients (OR, 3.24; 95% CI, 2.13–4.92).
Low-quality evidence from 13 observational studies3–7,11,17,19,22,28–31 enrolling 95354 patients found improved ROSC in EMS systems with a PAD program compared with systems without a PAD program (OR, 2.45; 95% CI, 1.88–3.18).
These recommendations were created by the AHA Adult Basic and Advanced Life Support Writing Group and are supported by a 2020 ILCOR systematic review.33
| COR | LOE | Recommendation |
|---|---|---|
| 2a | B-NR |
|
Synopsis
Despite the recognized role of lay first responders in improving OHCA outcomes, most communities experience low rates of bystander CPR8 and AED use.1 Mobile phone technology, such as text messages and smartphone applications, is increasingly being used to summon bystander assistance to OHCA events. For example, some smartphone apps allow emergency dispatch telecommunicators to send out alerts to CPRtrained community members who are within close proximity to a cardiac arrest event and use mapping technology to guide citizens to nearby AEDs and cardiac arrest victims.2
An ILCOR systematic review10 found that notification of lay rescuers via a smartphone app or text message alert is associated with shorter bystander response times,2 higher bystander CPR rates,5,6 shorter time to defibrillation,1 and higher rates of survival to hospital discharge3–5,7 for individuals who experience OHCA. Technology currently exists for emergency dispatch systems to use mobile phone technology to summon willing bystanders to nearby events where CPR and/or defibrillation may be required. As these technologies become more ubiquitous, they are likely to play an expanding role in the Chain of Survival. Randomized controlled trials, cost-effectiveness studies, and studies exploring this intervention for diverse patient, community, and geographical contexts are required. The psychological impact of engaging citizens to provide care to bystanders is unclear.
Recommendation-Specific Supportive Text
- A systematic review9 identified 1 RCT6 and 6 observational studies1–5,7 reporting uniformly positive data supportive of using mobile phone technology to summon bystanders. Meta-analysis of 4 observational studies enrolling 2905 OHCA events showed improvement in survival to hospital discharge when a citizen responder was notified of an OHCA by mobile phone technology (adjusted relative risk [aRR], 1.70; 95% CI 1.16–2.48) compared to no notification.3–5,7 This evidence is of low certainty due to the biases inherent in observational work. One RCT6 enrolling 667 patients with OHCA found that bystander CPR rates were increased by 14% (aRR, 1.27; CI 1.10– 1.46) when citizen responders were notified by mobile phone technology, although ROSC and survival were not increased. An observational study of 1696 OHCA events reported an increase of 16% in bystander CPR rate (aRR, 1.29; CI 1.20–1.37) when lay rescuers were notified via text message.5 Four observational studies including 1833 OHCA episodes showed that lay rescuers notified by mobile phone technology arrived between 3 and 4 minutes faster than ambulances.1–3,7 Time to defibrillation was reduced by 2 minutes and 39 seconds when citizens were notified via text message to bring an AED compared with ambulance response.1 No study reported the occurrence of any adverse events related to citizen notification. To date, there have been no studies conducted in North America, and important cultural and geographic differences could alter the effect of these technologies between countries and regions. Further studies are required to establish efficacy.
These recommendations were created by the AHA Resuscitation Education Science Writing Group and are supported by a 2020 ILCOR systematic review.10
Introduction
Early, effective bystander CPR is a critical component of the OHCA Chain of Survival. Unfortunately, rates of bystander CPR remain low for both adults and children. As the initial public safety interface with the lay public in a medical emergency, telecommunicators are a critical link in the OHCA Chain of Survival. In adults and children with OHCA, the provision of CPR instructions by emergency telecommunicators (commonly called call takers or dispatchers) is associated with increased rates of bystander CPR and improved patient outcomes. EMS systems that offer telecommunicator CPR instructions (T-CPR; sometimes referred to as dispatcher-assisted CPR, or DA-CPR) document higher bystander CPR rates in both adult and pediatric OHCA.1–3 Unfortunately, bystander CPR rates for pediatric OHCA remain low, even when T-CPR is offered. The T-CPR process should be scripted to maximize the number of OHCA victims receiving bystander CPR, and quality improvement mechanisms should be used routinely.
Because the evidence base for this question is distinct for adult and pediatric patient populations, the AHA Adult Basic and Advanced Life Support Writing Group and the AHA Pediatric Basic and Advanced Life Support Writing Group performed separate reviews.
| COR | LOE | Recommendations |
|---|---|---|
| 1 | C-LD | |
| 2a | C-LD |
Recommendation-Specific Supportive Text
- A telecommunicator receiving an emergency call for service (ie, a 9-1-1 call) for an adult patient in suspected cardiac arrest first should acquire the location of the emergency so that appropriate emergency medical response can be dispatched simultaneous to OHCA identification.1 Asking the 2 scripted questions from the No-No-Go process (Figure 3) to determine if a victim is unresponsive with abnormal breathing may positively identify up to 92% of people suffering OHCA.2
- When a caller describes an adult victim as unresponsive, with absent or abnormal breathing, telecommunicators should conclude that the victim is experiencing OHCA and should immediately provide T-CPR instructions.3,5 To address the variation in OHCA presentations, telecommunicators should be trained to identify OHCA across a broad range of circumstances, including agonal gasping and brief myoclonus.4
These recommendations were created by the AHA Adult Basic and Advanced Life Support Writing Group and are supported by the “2019 AHA Focused Update on Systems of Care: Dispatcher-Assisted CPR and Cardiac Arrest Centers: An Update to the AHA Guidelines for CPR and ECC,” a 2018 ILCOR systematic review, and a 2020 AHA statement.3,5,6
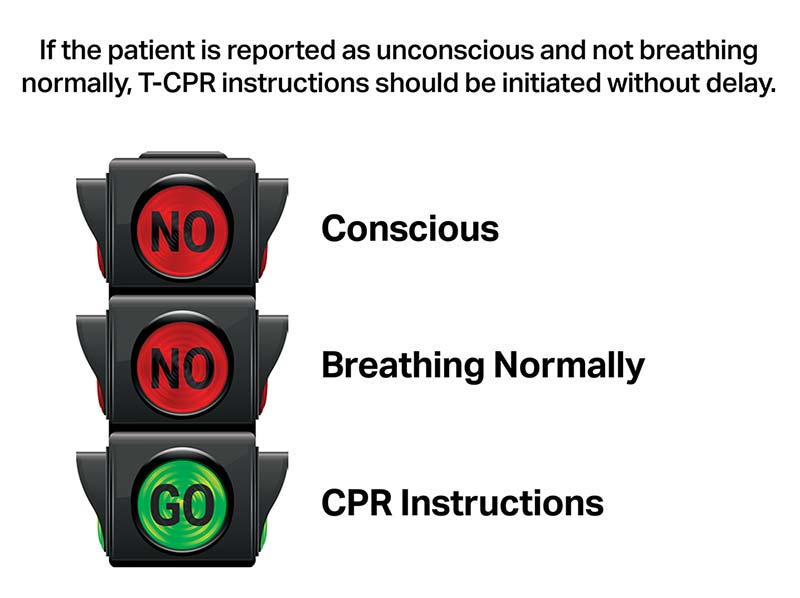
From The Road to Recognition and Resuscitation: The Role of Telecommunicators and Telephone CPR Quality Improvement in Cardiac Arrest Survival. With permission from The Resuscitation Academy, Seattle, WA. CPR indicates cardiopulmonary resuscitation; and T-CPR, telephone cardiopulmonary resuscitation.
| COR | LOE | Recommendations |
|---|---|---|
| 1 | C-LD |
|
| 1 | C-LD |
|
| 1 | C-LD |
|
Recommendation-Specific Supportive Text
- Early access to EMS via emergency dispatch centers (ie, 9-1-1) and early CPR are the first 2 links in the Chain of Survival for adult OHCA. In 3 adjusted observational studies, T-CPR was associated with a greater than 5-fold likelihood of provision of bystander CPR,8–10 and CPR was initiated 7 minutes sooner9 compared with no T-CPR.
- The delivery of bystander CPR before the arrival of professional responders is associated with survival and favorable neurological outcome in 6 observational studies.8,9,11–14 In 2 studies, offering T-CPR was associated with increased survival with favorable neurological outcome at 1 month after discharge, even after adjustment for multiple variables.9,12 Therefore, every emergency communications center should provide timely T-CPR instructions in all calls in which an OHCA victim is identified.3
- Based on meta-analysis of the 2 largest randomized trials comparing dispatcher compression-only CPR with conventional CPR (total n=2496), dispatcher instruction in compression-only CPR was associated with long-term survival benefit compared with instruction in chest compressions and rescue breathing.6,15
Recommendation-Specific Supportive Text
- Successful T-CPR programs should have a robust quality improvement process, including auditory review of OHCA calls, to ensure that T-CPR is being provided as broadly, rapidly, and appropriately as possible.16,17
These recommendations were created by the AHA Adult Basic and Advanced Life Support Writing Group and are supported by the “2019 AHA Focused Update on Systems of Care: Dispatcher-Assisted CPR and Cardiac Arrest Centers: An Update to the AHA Guidelines for CPR and ECC”; a 2018 ILCOR systematic review; and a 2020 AHA statement.3,5,6
| COR | LOE | Recommendations |
|---|---|---|
| 1 | C-LD |
|
| 1 | C-LD |
|
Recommendation-Specific Supportive Text
- A recent ILCOR systematic review provides evidence that T-CPR is associated with improved patient outcomes in children and adults compared to no T-CPR.6 An observational study reported the association of T-CPR with increased survival at 1 month in children with OHCA.1 An observational study of 5009 cardiac arrest patients showed that offered dispatcher-assisted CPR was associated with improved 1-month survival but not with 1-month favorable neurological outcome. The provision of bystander CPR, with or without dispatcher instruction, was associated with improved odds of survival and survival with favorable neurological outcomes compared with no bystander CPR.2
- A cross-sectional registry study demonstrated that both T-CPR and unassisted bystander CPR were associated with increased likelihood of favorable neurological outcome at hospital discharge compared with no bystander CPR.3 A more recent cross-sectional study of children with OHCA from the same database noted the association of bystander CPR with more than double the survival with favorable neurological function at hospital discharge, whether that bystander CPR was delivered with or without dispatcher assistance.4
These recommendations were created by the AHA Pediatric Basic and Advanced Life Support Writing Group and are supported by the “2019 AHA Focused Update on Pediatric Basic Life Support: An Update to the AHA Guidelines for CPR and ECC” and a 2019 ILCOR systematic review.6
Survival from IHCA remains variable, particularly for adults.1 Patients who arrest in an unmonitored or unwitnessed setting, as is typical on most general wards, have the worst outcomes. Outcomes from pediatric IHCA have improved, and survival rates are as high as 38%,2 and most pediatric IHCAs occur in ICUs.3 In-hospital cardiac or respiratory arrest can potentially be prevented by systems that recognize and dedicate resources to the deteriorating patient. MET or RRT activation by the bedside care team or family members ideally occurs as a response to changes noted in a patient’s condition. These teams respond to patients with acute physiological decline in an effort to prevent in-hospital cardiopulmonary arrest and death. Although rapid response systems have been widely adopted, outcome studies have shown inconsistent results. The composition of the responding teams, the consistency of team activation and response, as well as the elements comprising the early warning scoring systems vary widely between hospitals, thus making widespread scientific conclusions on the efficacy of such interventions difficult.
Because the evidence base for this question is distinct for adult and pediatric patient populations and pediatric patient populations, the AHA Adult Basic and Advanced Life Support Writing Group and the AHA Pediatric Basic and Advanced Life Support Writing Group performed separate reviews.
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD |
|
| 2b | C-LD |
|
Recommendation-Specific Supportive Text
- A recent ILCOR systematic review found inconsistency in the results of observational studies of RRT/MET system implementation, with 17 studies demonstrating a significant improvement in cardiac arrest rates and 7 studies finding no such improvement.1 One large RCT demonstrated no benefit in cardiac arrest occurrence or mortality.2 On the basis of this evidence, it appears that implementation of an RRT/MET system can be effective in decreasing non-ICU cardiac arrests, and possibly mortality, but further evaluations are necessary. Higher-intensity systems (eg, higher RRT/MET activation rates, senior medical staff on RRTs/METs) appear to be more effective. Heterogeneity in study design, context, patient populations, response team composition, team activation criteria, and outcomes studied prevent critical analysis of data across studies.
- The systematic review focused primarily on the effect of RRT/MET systems, but the use of early warning systems was also included. No RCTs were identified on the use of early warning scoring systems with the specific goal of decreasing adult IHCA. One observational study was included, which found that the Modified Early Warning Score had an inconsistent ability to predict IHCA.1,3 More recently, there is growing interest in machine learning and other approaches to aid in early detection of deterioration, and further study of these is warranted.4
These recommendations were created by the AHA Adult Basic and Advanced Life Support Writing Group and are based on a 2020 ILCOR systematic review that focused on RRT/MET implementation.1
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD |
|
| 2b | B-R |
Recommendation-Specific Supportive Text
- RRT/MET systems are associated with reductions in hospital mortality and cardiopulmonary arrest rates in both adult and pediatric populations.1–3 One observational registry study of 38 pediatric hospitals found no difference in risk-adjusted mortality rates associated with RRT/MET implementation.4 There is low-quantity and low-quality evidence evaluating the role of RRT/MET systems to prevent pediatric cardiac arrest. Major limitations are the low rate of pediatric cardiac arrests and mortality (especially outside the ICU setting) and the heterogeneity of the patient populations.
- In a multicenter, international cluster randomized trial, implementation of the bedside pediatric early warning system was associated with a decrease in clinically important deteriorations on the wards of nontertiary care in community hospitals, but not with all-cause mortality.5 Four recent systematic reviews and 1 recent scoping review found limited evidence that the use of the pediatric early warning system leads to reductions in deterioration.1,6–9 One scoping review found evidence, though limited, suggesting that the pediatric early warning system is useful in low- or middle-income countries.8
These recommendations were created by the AHA Pediatric Basic and Advanced Life Support Writing Group and are based on a 2019 ILCOR scoping review and a 2020 evidence review.10
| COR | LOE | Recommendations |
|---|---|---|
| 2b | C-LD |
|
| 2b | C-LD |
|
Synopsis
Cognitive aids improve patient care in nonacute settings,10,11 yet little is known of their impact in critical situations. Understanding if, when, and how cognitive aids can be useful may help improve the resuscitation efforts of lay providers and healthcare professionals, thereby saving more lives. We considered cognitive aids as a “presentation of prompts aimed to encourage recall of information in order to increase the likelihood of desired behaviors, decisions, and outcomes.”12 Examples include checklists, alarms, mobile applications, and mnemonics.
An ILCOR systematic review suggests that the use of cognitive aids by lay rescuers results in a delay in initiating CPR during simulated cardiac arrest, which could potentially cause considerable harm in real patients.14 The use of cognitive aids for lay providers during cardiac arrests requires additional study before broad implementation. No studies were identified evaluating the use of cognitive aids among healthcare teams during cardiac arrest. Evidence from trauma resuscitation suggests that the use of cognitive aids improves adherence to resuscitation guidelines, reduces errors, and improves survival of the most severely injured patients. It may be reasonable for healthcare providers to use cognitive aids during cardiac arrest. Extrapolation from a closely related field is appropriate but requires further study. Future research should explore whether cognitive aids support the actions of bystanders and healthcare providers during actual cardiac arrests.
Recommendation-Specific Supportive Text
- Results from a systematic review14 identified 4 randomized trials1–4 demonstrating a statistically significant and clinically relevant delay in initiating CPR when lay rescuers used cognitive aids (30-second–70-second difference between groups in each study). Once CPR is initiated, rescuers who are using cognitive aids appear to have less hands-off time1,2,4,5 and are more confident in their ability to act,4 which may ultimately be important to support a lay provider in responding to a cardiac arrest.
- The systematic review identified no studies analyzing survival to discharge using cognitive aids in cardiac arrest, but it did identify 3 studies related to trauma resuscitation, including 1 RCT6 and 2 observational studies.7,9 Survival to hospital discharge was higher in the observational studies for those with the most significant injury (Injury Severity Score 25 or greater) when a cognitive aid was used.7,9 The RCT included patients with lower injury severity and did not demonstrate a difference in survival.6 Measures of resuscitation performance (eg, fewer errors, completion of primary and secondary surveys, quicker performance of tasks), although inconsistently used as metrics in each study, generally favored the use of cognitive aids in trauma resuscitation.6–9
These recommendations were created by the AHA Resuscitation Education Science Writing Group and are supported by a 2020 ILCOR systematic review.14
| COR | LOE | Recommendation |
|---|---|---|
| 2a | C-LD |
|
Synopsis
Cardiac arrest centers (CACs), although still lacking official criteria for designation as has been established for other centers of expertise, are specialized facilities that provide comprehensive, evidence-based post–cardiac arrest care, including emergent cardiac catheterization, targeted temperature management, hemodynamic support, and neurological expertise. A CAC may also have protocols and quality improvement programs to ensure guideline-compliant care. A growing number of CACs also have the capability to provide extracorporeal membrane oxygenation and/or other forms of circulatory support. Patients may be transported directly to CACs by EMS either during resuscitation or after ROSC, or they may be transferred from another hospital to a CAC after ROSC. Important considerations in this decision- making process must include transport time, the stability of the patient, and the ability of the transporting service to provide needed care.
Although supportive evidence for comprehensive post–cardiac arrest interventions remains largely observational (particularly when they are administered together as bundled care at specialized centers) and the results of these studies are mixed, CACs may nonetheless represent a logical clinical link between successful resuscitation and ultimate survival. Taken together with experience from regionalized approaches to other emergencies such as trauma, stroke, and ST-segment elevation acute myocardial infarction, when a suitable complement of post–cardiac arrest services is not available locally, direct transport of the resuscitated patient to a regional center offering such support may be beneficial and is a reasonable approach when feasible.
Recommendation-Specific Supportive Text
- Evidence-based, comprehensive post–cardiac arrest care is critically important for resuscitated patients. The adjusted analyses from 2 observational studies found that treatment at CACs was not associated with increased survival with favorable neurological outcome at 30 days,2,3 whereas 2 other studies found that admission to a CAC was associated with improved survival to hospital discharge with good neurological outcome.4,7 Treatment at CACs was associated with increased 30-day survival5,6 and survival to hospital discharge4,7–10 compared with treatment at non-CACs. An interim feasibility report (n=40 patients) of a randomized trial evaluating expedited transport to a CAC demonstrated no difference in clinical outcomes, but it is preliminary and underpowered for this outcome.11
These recommendations were created by the AHA Adult Basic and Advanced Life Support Writing Group and are supported by a 2019 ILCOR systematic review.12
| COR | LOE | Recommendations |
|---|---|---|
| 1 | B-NR |
|
| 2b | B-NR |
|
Synopsis
Organ donation can occur after death by neurological criteria or after death by circulatory criteria. Donation after circulatory death may occur in controlled and uncontrolled settings. Controlled donation after circulatory death usually takes place in the hospital after withdrawal of life support. Uncontrolled donation usually takes place in an emergency department after exhaustive efforts at resuscitation have failed to achieve ROSC. Organ donation in any setting raises important ethical issues. Decisions for termination of resuscitative efforts or withdrawal of life-sustaining measures must be independent from processes of organ donation.
In 2015, the ILCOR Advanced Life Support Task Force reviewed the evidence for the impact that a donor having received CPR has on graft function. The 2 general comparisons were 1) controlled organ donation using organs from a donor who had previously received CPR and obtained ROSC compared with a donor who had not received CPR and 2) uncontrolled donation using organs from a donor receiving ongoing CPR, for whom ongoing resuscitation was deemed futile, compared with other types of donors,1 on the question of whether an organ retrieved in the setting of controlled donation versus uncontrolled donation had an impact on survival and complications.
Recommendation-Specific Supportive Text
1 and 2. Studies comparing transplanted organ function between organs from donors who had received successful CPR before donation and organs from donors who had not received CPR before donation have found no difference in transplanted organ function.2–6 Outcomes studied include immediate graft function, 1-year graft function, and 5-year graft function. Studies have also shown no evidence of worse outcome in transplanted kidneys and livers from adult donors who have not had ROSC after CPR (uncontrolled donation) compared with those from other types of donors.7–9 There is broad consensus that decisions for termination of resuscitative efforts and the pursuit of organ donation need to be carried out by independent parties.10–13
These recommendations were created by the AHA Adult Basic and Advanced Life Support Writing Group and are supported by a 2015 systematic evidence review.1,14 A comprehensive ILCOR review is anticipated in 2020.
| COR | LOE | Recommendations |
|---|---|---|
| 2a | B-NR |
|
| 2a | B-NR |
|
| 2a | B-NR |
|
| 2a | C-EO |
|
Synopsis
Post-event debriefing is defined as “a discussion between 2 or more individuals in which aspects of performance are analyzed,”6 with the goal of improving future clinical practice.7 During debriefing, resuscitation team members may discuss process and quality of care (eg, algorithm adherence), review quantitative data collected during the event (eg, CPR metrics), reflect on teamwork and leadership issues, and address emotional responses to the event.8–13 A facilitator, typically a healthcare professional, leads a discussion focused on identifying opportunities and strategies for improving performance.8,9,11,13,14 Debriefings may occur either immediately after a resuscitation event (hot debriefing) or at a later time (cold debriefing).7,9,15 Some debriefings take the form of personalized reflective feedback conversations,1,4 while others involve group discussion among a larger, multidisciplinary resuscitation team.2,3 We examined the impact of postevent clinical debriefing on process measures (eg, CPR quality) and patient outcomes (eg, survival). Studies related to critical incident stress debriefing (ie, psychological debriefing), which is a process intended to prevent or limit post-traumatic stress symptoms, were excluded from the review but have been well reviewed elsewhere.16 Data-informed debriefing of providers after cardiac arrest has potential benefit for both in-hospital and out-of-hospital systems of care; discussion should ideally be facilitated by healthcare professionals.1–4
Recommendation-Specific Supportive Text
- One prospective, observational study of post- OHCA debriefing among prehospital personnel demonstrated improved quality of resuscitation (ie, increased chest compression fraction, reduced pause duration) but no improvement in survival to discharge.1 Good and poor performance were highlighted during discussion.
- Three prospective observational studies of post- IHCA debriefing among multidisciplinary resuscitation team members show mixed results.2–4 Meta-analysis of these studies demonstrated improved ROSC and mean chest compression depth in the period after implementation of debriefing. Two studies demonstrating improvements in quality of resuscitation (ie, chest compression depth, chest compression fraction, pause duration, excellent CPR) and survival outcomes (ie, ROSC, survival with favorable neurological outcome),2,3 and 1 study demonstrated no improvement in patient or process-focused outcomes.4
- Because provider recall of events and self-assessment of performance are often poor,9,17,18 debriefings should be supplemented by discussion of objective, quantitative data such as CPR quality performance data (chest compression rate, depth, and fraction; telemetry and defibrillator tracings; end-tidal CO2 tracings; and resuscitation records.1–4
- In all studies reviewed, debriefings were facilitated by healthcare professionals familiar with the recommended debriefing process or structure, which in some cases was supported by the use of a cognitive aid or checklist.1–4 Discussions were tailored to participant type and group size and were individualized to the nature of performance during the event.
These recommendations were created by the AHA Resuscitation Education Science Writing Group and are supported by a 2019 ILCOR systematic review.19
| COR | LOE | Recommendation |
|---|---|---|
| 2a | C-LD |
|
Synopsis
Many industries, including healthcare, collect and assess performance data to measure quality and identify opportunities for improvement. This can be done at the local, regional, or national level through participation in data registries that collect information on processes of care (CPR performance data, defibrillation times, adherence to guidelines) and outcomes of care (ROSC, survival) associated with cardiac arrest. The AHA’s Get With The Guidelines–Resuscitation registry is one such initiative to capture, analyze, and report processes and outcomes for IHCA.
A recent ILCOR systematic review7 found that most studies assessing the impact of data registries, with or without public reporting, demonstrate improvement in cardiac arrest survival outcomes after the implementation of such systems.1–6,8–21 Although hospitals act on recorded metrics in other situations, it is unclear what exact changes are made in response to these analytics. The collection and reporting of performance and survival data and the implementation of performance improvement plans, with or without public reporting of metrics, may lead to improved systems performance and, ultimately, benefit patients. Use of registries to target interventions for communities with particular need is of interest, and further study is needed to inform optimal implementation strategies of such systems in the future.
Recommendation-Specific Supportive Text
- A recent ILCOR systematic review7 found 6 observational studies demonstrating that the implementation of cardiac arrest registry was associated with improved survival and adherence to key performance indicators (CPR process measures, time to defibrillator application, adherence to guidelines) over time.1–6
In an observational study of a registry that included 104 732 patients with IHCA, for each additional year of hospital participation in the registry, survival from cardiac arrest increased over time (OR, 1.02 per year of participation; CI, 1.00–1.04; P=0.046).1 Another observational study of a multistate registry included 64 988 OHCA and found that all‐rhythm survival doubled (8.0% preregistry, 16.1% postregistry; P<0.001) after registry implementation.6 A state OHCA registry enrolling 15 145 patients found improved survival to hospital discharge (8.6%–16%) over the 10-year study period.5 In another study that included a state registry of 128 888 OHCAs that mandated public reporting of outcomes, survival increased over a decade from 1.2% to 4.1%.4
These recommendations were created by the AHA Resuscitation Education Science Writing Group and are supported by a 2020 ILCOR systematic review.7
Resuscitation science, including understanding about integrated systems of care, continues to evolve. Among the many high-priority unresolved questions are the following:
- Although the clinical effectiveness of community CPR and AED programs is well established, the populations and settings in which these interventions are cost-effective requires further study.
- Preliminary studies of drone delivery of AEDs are promising.1,2 Given the time-sensitive benefit to defibrillation, this concept and other means for just-in-time AED delivery deserve further study.
- The RRT/MET concept seems promising, but current data are too heterogeneous to support strong conclusions. Systematic data collection would greatly improve understanding of the types of interventions and characteristics of patients who benefit from RRT/MET interventions as well as the makeup and activities of successful teams.
- Along the same lines, validated clinical criteria, perhaps developed by machine-learning technology, may have value to identify and direct interventions toward patients at risk of IHCA.
- Although the concept is logical, cognitive aids (other than T-CPR) to assist bystanders in performing CPR have not yet proven effective. Given the ubiquity of smartphones and the innovation of smartphone app platforms, additional study is warranted.
- Low rates of bystander CPR persist for women, children, and members of minority communities. Efforts to improve bystander response in these populations should be implemented and evaluated for effectiveness.
- Creating a culture of action is an important part of bystander response. More research is needed to understand what key drivers would influence bystanders to perform CPR and/or use an AED.
- Additional research is needed on cognitive aids to assist healthcare providers and teams managing OHCA and IHCA to improve resuscitation team performance.
- Although the value of immediate feedback (eg, team debriefing) and data-driven systems feedback is well established, specific high-yield components of that feedback have yet to be identified.
- More research is needed to better understand how to use technology to drive data and quality improvement both inside and outside of the hospital for cardiac arrest patients.
The American Heart Association requests that this document be cited as follows: Berg KM, Cheng A, Panchal AR, Topjian AA, Aziz K, Bhanji F, Bigham BL, Hirsch KG, Hoover AV, Kurz MC, Levy A, Lin Y, Magid DJ, Mahgoub M, Peberdy MA, Rodriguez AJ, Sasson C, Lavonas EJ; on behalf of the Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, and Resuscitation Education Science Writing Groups. Part 7: systems of care: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142(suppl 2):S580–S604. doi: 10.1161/CIR.0000000000000899
- Katherine M. Berg, MD, Chair
- Adam Cheng, MD
- Ashish R. Panchal, MD, PhD
- Alexis A. Topjian, MD, MSCE
- Khalid Aziz, MBBS, BA, MA, MEd (IT)
- Farhan Bhanji, MD, MSc (Ed)
- Blair L. Bigham, MD, MSc
- Karen G. Hirsch, MD
- Amber V. Hoover, RN, MSN
- Michael C. Kurz, MD, MS
- Arielle Levy, MD, MEd
- Yiqun Lin, MD, MHSc, PhD
- David J. Magid, MD, MPH
- Melissa Mahgoub, PhD
- Mary Ann Peberdy, MD
- Amber J. Rodriguez, PhD
- Comilla Sasson, MD, PhD
- Eric J. Lavonas, MD, MS
On behalf of the Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, and Resuscitation Education Science Writing Groups
The authors thank Dr Monica Kleinman for her contributions.
Open table in a new window.
Open table in a new window.
 Login
Login
